McKenna's Birth Story
McKenna’s birth was long awaited in many ways. After experiencing birth trauma in the hospital setting with my first two, I was determined to find a way to experience beauty within the realm of birth. I knew I couldn’t do this by returning to the place of my traumas, so I started looking into alternate locations to deliver her. While I was most comfortable delivering at a birth center, I was quickly turned away by all of the local centers due to having a c-section in my history with my firstborn. It was then that I turned towards finding a midwife and making preparations for a homebirth.
The next nine months were full of mental, physical, and spiritual preparation. I wanted to make sure I was doing everything in my power to make this birth different. I emphasized a healthy diet and stayed on top of my physical health. I spoke with my therapists to work through my previous traumas. I watched countless videos of successful homebirths. I worked on birth meditation and becoming in-tune with my mind-body connection. I got weekly chiropractic. And among other things, I prayed over this birth daily.
As if my anticipation for this birth wasn’t enough, McKenna gave us her first surprise by deciding to be the first of our children to come after their due date. For nine months, I expected her to arrive early, just as our other two had. But she stayed nice and comfortable until 40+4 weeks gestation. On the morning of October 30th, I was awoken several times by strong contractions in my back. At around 6:00am, I decided to get up and pay closer attention to whether or not this may be the first signs of labor. The contractions continued, strong but manageable, and were consistent enough that I decided to text all of my support team. By 6:30am everyone had been informed of my labor signs and were starting to prepare their things to head over upon my request.
I spent the entirety of early labor working through contractions on my bed. Bobby applied counter-pressure on my back while I kept a timer. Our support team began to arrive one at a time - first my parents to help with the older kids, then my friend who was photographing the birth for us, then my doula, and eventually, once she was needed, my midwife and her secondary support midwife.
Although contractions were picking up in intensity and time, I felt very in control. I was breathing and vocalizing through them well while Bobby and my doula, Amanda, took turns applying counter-pressure. As my older two kids woke up, they each came in to visit me and held my hand through a few contractions. We chatted briefly about the excitement of their baby sister coming and I gave them each a kiss before telling them to go spend some time with their Dedaw.
My mom came in and sat on the bed beside me. I could see the emotion welling up in her eyes as she watched her little girl working hard to bring her granddaughter into this world. As an adopted child, one of my greatest joys in McKenna’s birth plan was to give my mom the opportunity to witness birth firsthand. What a privilege it was to get to labor with her energy in the room.
Sometime around 9:30am I could tell the contractions were nearing their peak intensity. The birth tub was filled and ready so I decided to move from my bed and into the birthing pool. Almost immediately after doing so, my contractions switched into what was clearly transition. Fortunately, transition moved quickly and after only a few contractions, my body began to show signs of wanting to bear down. Around 10:00am I started pushing.
I pushed for what I’m guessing was about 45 minutes before I started to hear people begin to prepare for her arrival. My birth team turned off our ceiling fan to keep her warm, talked to Bobby about his jobs when she came out, and instructed me that she should be joining us in the next couple of pushes. I gathered myself as best I could and gave the next few contractions the strongest pushes I could muster. But she didn’t come.
Contraction after contraction, I would bear down but it was clear that something was wrong. She was no longer progressing in the way that we had expected. My midwife, Elise, informed me that sometimes a baby can get caught on a piece of the cervix that is still present, called a cervical lip. I agreed to let her manually lift the cervical lip over McKenna’s head in hopes that would clear the path for her to finish her descent through the birth canal. Elise did this swiftly, but unfortunately it caused them to become aware that McKenna was out of position. She was turned posterior - the same as her brother six years prior that caused me to need a c-section.
At this point the midwives and doula began walking me through multiple different techniques to try to get her turned. For each of them, I was instructed to do my best to keep from pushing during each contraction, something I’ve since determined may be the most physically painful human experience. I focused, rather unsuccessfully, to fight my body’s urge to push as we moved through different positions - first in the tub, then on the bed, and finally on the birthing ball. After each one they’d allow me to bear down for a few contractions to see if it had made a difference for McKenna, and each time it was determined unsuccessful.
As time continued to tick on and interventions continued to fall short, I became acutely aware of my energy levels. I realized that there was a very real possibility that we may need a different exit plan, and I needed to be sure to save just enough energy to get me and McKenna safely to a hospital. I trudged on for about another hour, praying with each push that it’d be the one to get her to descend the fraction more that she needed to finally join us earthside. But it was to no avail.
Finally around 1:00pm, with the midwives still equipped with a couple more tools in their toolbox, I turned to Elise and told her that we needed to transfer to a hospital. It was time. My tank was nearly on empty and I knew I still had to make it to the hospital and be successfully admitted and prepped before I would get any relief. They asked if I was sure and told me we still had a few things we could try at home. I let them know that I truly had nothing more to give, and informed them that I desired to request a c-section at the hospital. As much as I had wanted a vaginal delivery, I couldn’t imagine pushing any more than I already had to, even with an epidural in my system.
Bobby and the team quickly prepped for a hospital transfer. They threw a few necessities into a makeshift hospital bag and I screamed my way through contractions and into Bobby’s car. We drove the 5 minutes it takes us to get to the closest hospital. While it wasn’t our hospital of choice, it was by far the closest, and at this point, my biggest concern was getting her out of me and finding relief as quickly as possible.
As we pulled up to the hospital the emergency room doors were open. I was mid-contraction when Bobby opened my door. At this point, I was far beyond being able to have any sort of calm or control over my contractions. I had reached the end of my energy reserve and my body was responding purely primally, yelling and writhing through each one. As I slowly moved out of the car mid-scream, not a single one of the emergency room staff moved to get a wheelchair or assist in anyway.
Rather shocked, I mentally noted the difference in care I was about to receive between the homebirth experience and what we were walking into at the hospital and I tried to prepare myself. Finally, once I walked myself inside with Bobby’s support, looked at someone dumbfounded and stated “We need a wheelchair,” and had another painful contraction in the lobby, someone finally came in with the chair I requested. They hurriedly wheeled me up to the delivery floor where they began to prep me for a c-section.
What transpired for the next thirty minutes truly makes me shake my head in disbelief. It was as though none of the hospital staff had ever dealt with a contracting mother before. By this time, intense contractions were coming every couple of minutes. They’d hang around for 45 seconds or so, in which I would scream and writhe in pain, and then I’d have a minute or so break before another one took over my body. A nurse came into my room with an intake form and the doctor came in the assess the situation. She stayed for no more than 30 seconds before she mumbled a few lines of medical jargon to her associate and then walked out. Even if I could understand what they were saying, I was mid-contraction, so I had no coherent awareness. My contraction fades, and the nurse takes this quiet moment to scribble a few notes on her papers. Then, just as another contraction is starting, she decides to continue the intake form. “Have you been vaccinated for COVID-19,” she asks. I scream, writhe. “So is that a yes, or…,” she prods, clearly annoyed. This lady cannot seriously expect me to form a verbal response in the middle of a 10cm contraction. At my bedside, Elise picks up on the absurdity of this all. She sternly lets the lady know that she’s going to have to wait a few seconds for the contraction to pass if she expects me to answer.
She waits a few seconds until I’m able to cooperate with her questioning. Then she proceeds to ask me to sign a form that gives them permission to give me anesthesia and put me under for the c-section. Confused, I tell her that I don’t want to be asleep for McKenna’s birth. Cue another contraction. “You don’t have a choice,” she tells me. One of the big lies hospitals will voice. You always have a choice. Elise’s mama-bear senses kick in again and she begins to advocate for me while I work through my screaming and writhing routine on the bed. “You need to get the doctor back in here and fully explain to her what her options are and why you’re suggesting she gets put under. If that’s not what she wants, she definitely doesn’t need to. But you can’t just walk in here and throw around medical jargon in the middle of a contraction and then ask an uninformed patient to sign some forms that she doesn’t understand.” Boom.
I’ll be honest, even while experiencing contractions, watching a midwife lecture hospital staff about improper patient treatment is quite gratifying. The doctor came in and began to directly and efficiently walk me through my options. She explained that the reason she wanted to put me under was because McKenna was too deep into the birth canal. In order to extract her from the incision, they’d need to manually push her back up the birth canal, which adds a significant complication to the surgery. She explained that she could do a spinal, but if for any reason it didn’t take, we’d have to wait to give a second dose, and then if for any reason there was still an issue, I could be awake for a very unpleasant procedure. Upon hearing this, I immediately recalled how my first spinal didn’t take with Beckett’s c-section, and how even after they administered a second, I could still feel pain during the operation. After being properly explained my options, and not wanting to risk having a spinal not take again given my history, I agreed to receive anesthesia.
Shortly after, I was wheeled into the operating room. I painfully moved onto the operation table with very little assistance from anyone in the room. I then continued to experience unbearable contractions while they prepped the room. At one point, they attempted to give me oxygen through a mask. It’s been a while since I’ve needed oxygen, so I can’t recall what it is supposed to feel like. But I can tell you this time it felt like the machine was turned off. They forcefully held it over my mouth and nose through my contractions while no air seemed to be coming through. I began to gasp for air as I was trying to work through my contractions. “I can’t breathe,” I’d panic. The response was a dismissive, “I know,” while continuing to hold the mask on my face. My annoyance for their lack of compassion around my contractions continued to skyrocket. Finally, they let me know that they’d be turning on the anesthesia and the next thing I remember is waking up back in a room with Bobby, Elise, and Amanda.
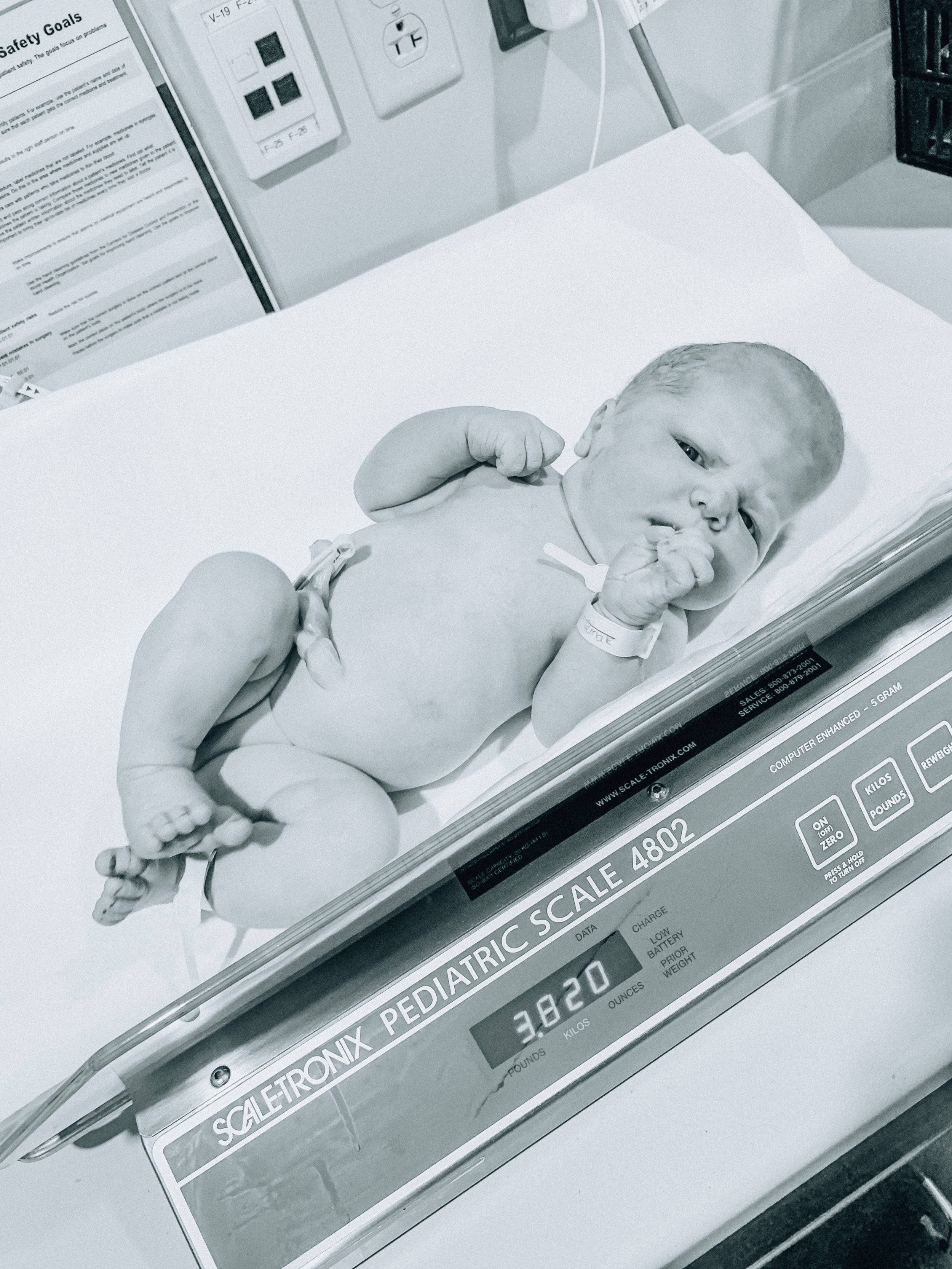
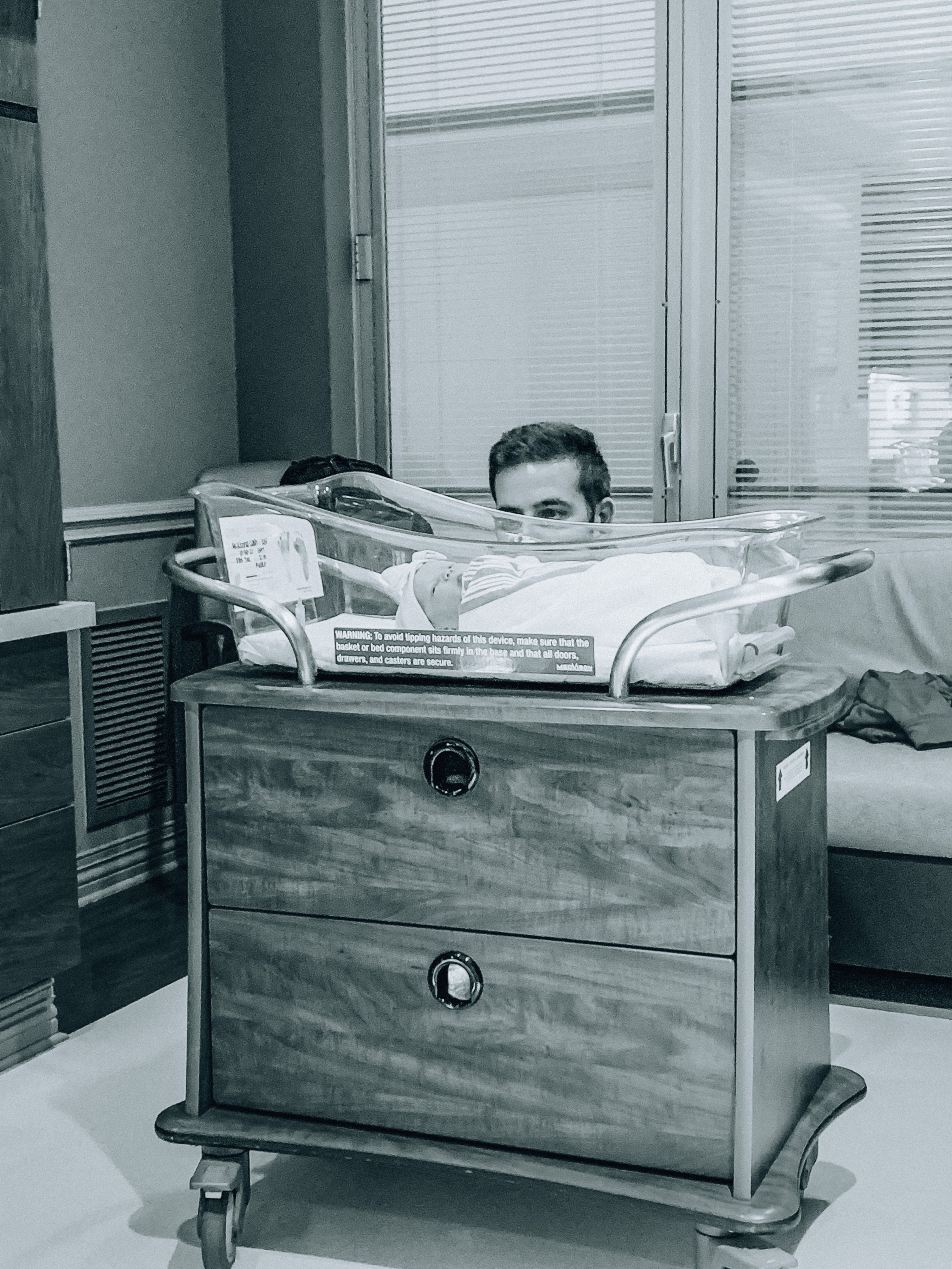
Once I awoke, they immediately brought McKenna over to me. She had been born at 1:47pm and weighed 8lbs 7oz with a massively protruding forehead from where she had gotten stuck in my birth canal. They laid her on my chest and I was overcome with a hazy relief and adoration for her. I made a mental note of how different the bonding experience was this time compared to my other two births. I don’t know if it’s because we knew she’d be the completion of our family, the fact that we’d put so much prayer into her birth being redemptive, or a combination of both, but meeting her seemed to have a spiritual divineness to it. After that, everything is a blur. I was weaning off the effects of the anesthesia and seemed to only be half aware as I laid in the room, with needles and tubes branching off of me in all directions. I don’t recall Elise or Amanda leaving and I also have no recollection of being moved into our overnight room. But eventually, we ended up there.
The first few hours were spent soaking up cuddles with our newborn. My next clear memory was being introduced to the night shift hospital staff. I was assigned a lovely older nurse named Joy, and McKenna was given a NICU nurse who happened to be working the nursery that evening. Shortly thereafter, the ugly flaws of the hospital system began to make their appearance. It started when McKenna’s nurse came in and began to tell us that McKenna was “LGA,” or large for her gestational age. “Excuse me?” I asked perplexed. “She is measuring large on our charts,” the nurse continued. I shook my head. “Respectfully, I don’t really care what your chart says. She’s 8lbs 7oz. That’s not an abnormally large size. Our other daughter who was born at 39 weeks weighed 8lbs 2oz. So considering McKenna stayed in my womb an extra week and a half, gaining a half pound more is right on track with where she should be. Even if 8’7” was large for the world’s standards, it’s not large for our family.” I was beginning to get frustrated. The nurse, unfazed and unswayed, continued down her LGA protocol. “We’re going to need to run a glucose test on her to make sure that it’s safe for her to be discharged.”
At this point I’m clearly annoyed and quite frankly confused. I’m looking at my perfectly healthy baby who is showing no signs of there being any problem, and yet we’re being seemingly forced into doing tests with no real justification as to why. I can’t stop thinking about the fact that if we were at home, like we had planned, no one would be bothering us for tests right now. I’d be laying in my bed, cuddling with my baby, uninterrupted. Instead, I’m worn out and recovering from a c-section that I had just a few hours prior, and having to battle it out with a rigid nurse who clearly lacked empathy. It’s an interesting thing being postpartum and post-op. In the past few years of working closely with women and hearing their birth experiences, I am rationally well aware that hospitals cannot do anything that we do not consent to. At the same time, it’s hard to prepare yourself for how quickly your exhausted rational brain will default to the road of least resistance when you’re in the middle of a recovery yourself. When this is paired with hospital staff that are more concerned with protocol than true informed consent, you’re left feeling utterly powerless. I thought about how badly I wanted to get home and how little energy I had to argue with her, and I agreed to them performing the glucose test. “What does it entail?” I asked. “It’s just a heal prick,” was her exact reply. “Fine.”
She began to prepare McKenna for a heal prick while explaining to me that she would need a score above a 45 to pass the glucose test. She asked me to feed her so that she was being tested immediately after a meal. Once I was finished nursing, the nurse came back in to prick McKenna’s heal, tested the blood, and reported back that McKenna had scored a 63. “Great, we’ll now have to test her 3 more times, but each of these will need to happen right before she eats. She’ll need to pass each one in order to be cleared for discharge.” WHAT?! The bullshit manipulation of this entire scenario had my blood boiling. I tried to keep a respectful tone in my voice as I continued to question why this test was even necessary in the first place. “It’s extremely important because glucose feeds the brain,” the nurse said repeatedly. In response, I kept gesturing towards McKenna, dumbfounded, and challenged, “Look at her! She’s fine! Her brain is fine! She is showing no signs of having any issues with her health.” She didn’t care. “We’ll be back right before the next feeding to test her. I need you to wait three hours between her feedings so we can test her at the right intervals.”
Apparently the absurdity of all of this was going to continue to escalate. Three hours?! We’re talking about a baby who is only a few hours old. She’s cluster feeding - or at least she should be. Never in my seven years of researching newborn care have I seen it recommended for a mother to wait three hours between feedings this soon after birth. Someone please point me to that study. The nurse left as my brain continued to spiral and I continued to become even more infuriated. But I did as she asked. Three hours later I called her in to the room so she could run her test and I could feed my baby. She tested her. 48. We passed. I grabbed McKenna and nursed her. “Call me back again in three hours before her next feeding.” Gugh.
When the nurse came in for the third test, it was clear to everyone that I wasn’t too fond of her current role in our lives or her approach to nursing care. Upon entering the room she exclaimed, “I know you’re not happy to see me but I’m here to do the next test.” She’s not wrong. Even still, I managed to stay respectful. Annoyed, but respectful. She pricked McKenna’s heal. “42.” Shit.
“She didn’t quite pass so we’re going to need to restart the tests from the beginning.” The nurse pulled out a tube of glucose and rubbed it all over McKenna’s gums. As I watch her, I’m beginning to feel like this whole experience is surreal. We need to restart from the beginning? So this little baby who my main wish for was zero intervention during and after birth, is now receiving countless heal pricks and ingesting a nasty tube of glucose that I don’t even know the ingredients of. The nurse continues, “You’re going to need to supplement with formula. She’s not getting enough from your breast milk.” What in the actual hell is happening? How quickly this has all spiraled out of control.
“What do you mean I need to supplement? She’s fine,” I argue. “You need to supplement,” the nurse repeats, “If she fails again I’ll have to take her to the NICU.” Completely dumbfounded at the idea of this, I question, “I’m sorry, you’re going to take a healthy 8lbs 7oz baby to the NICU? What are you talking about?” The nurse just looks at me. Once again, she’s unwavering in her nonsensical protocol. I continue, “So what are you going to do? Can you bring me a syringe or something so I can control how much I’m giving her?” “No,” she states matter of factly, “I’m going to bring you a bottle.” By now this nurse has to be so tired of me questioning everything, but I cannot get over how much this entire system lacks common sense. “A bottle?” I ask. “She’s a newborn. Her stomach is the size of a marble. Why would I need an entire bottle?” Out of annoyance I think she’s resorted to not answering me. She leaves the room to go collect my bottle.
I laid there venting to Bobby. All I could think about was how we were supposed to be at home right now. We were supposed to be laying in our bed with our baby without anyone giving us a hard time about unnecessary interventions. My midwives would have seen healthy vitals and normal behavior, and allowed us to enjoy those first few hours postpartum. But instead, here we were, trapped in a cold hospital system filled with outdated protocol and nonsensical systems. Our voices, humanity, and sense of empowerment had been stripped away. Stuck in a place where we are made to feel like what we want comes second to what the staff wants. Fortunately, God sent me an angel in the form of my nurse Joy that night. And she swooped in at just the right time.
Joy was standing outside my door when the nursery nurse returned holding a bottle of formula. Knowing I was a homebirth transfer, Joy seemed to have an inkling that this wasn’t going to go over well. She followed the nurse in. “What’s going on here?” Joy asked. The nursery nurse seemed surprised. “She needs to supplement with formula. The baby isn’t getting enough from breastmilk and she failed the glucose test. If she fails again she’ll have to go to the NICU.” The defensiveness was clear in her tone. Without missing a beat, Joy looked at her and asserted, “Have we even tried hand expressing yet? Or are you just jumping straight to formula?” Praise Jesus. A nurse that cares. A nurse that has compassion for my wishes. A nurse who’s willing to insert herself into a fight that I didn’t have the energy to take on myself. A nurse who wanted me to remember that I still had a voice in this hospital room. The nursery nurse seemed caught off guard but she stood her ground. “She needs to supplement. I’m already going against my supervisors wishes. My hands are tied.” I’m still not sure what this meant and looking back, I wish I would have pried more. Exactly how are you going against your supervisors wishes when I’ve done everything you’ve asked? But Joy quickly ushered her out of the room. “Fine, but leave the bottle of formula and me and mama are going to do this our way.” The level of comfort Joy brought me in such an undesirable situation is indescribable. Finally I felt like someone was in my corner in this cold and impersonal hospital.
The nursery nurse left and Joy looked at me and told me she was going to go get a syringe. I laughed and told her that I had asked for one in the first place. She rolled her eyes out of annoyance that I wasn’t given the very reasonable thing I had asked for. When she came back, we latched McKenna onto my breast and pulled a tiny 10cc of formula out of the bottle and into the syringe. As McKenna was nursing, Joy hand expressed my milk and slowly dripped formula into the corner of her mouth. As much as I wish we could’ve avoided formula altogether, I was so grateful that we could at least control the amount she was receiving, all while avoiding nipple confusion and encouraging nursing. It was making the best out of a crappy situation.
After this approach, McKenna tested well above the 45 count threshold. I was instructed to follow the same feeding method while the testing continued, except this time the tests would occur before the feedings at three hour intervals, just as they had before. The next feeding I was on my own for. I was significantly less skilled at hand expressing than Joy. I could tell McKenna wasn’t getting as much as she had before. By the time the test came around, three hours later, her numbers had dropped back in the upper 40’s. With only two tests left to pass, I refused to make us repeat this cycle again. I decided to ignore the instructions of the nurse and feed McKenna on demand. Screw this three hour nonsense. I fed her after an hour and a half and then again right before the three hour mark. The nurse came in shortly after I had finished and tested her. She passed. We repeated this for the fourth and final test of the series. She passed again. Thank God. The nursery nurse let me know that we wouldn’t need to test again unless McKenna showed signs of being lethargic. Why we couldn’t have just taken that approach in the first place is beyond me. I grabbed my baby, with cuts and bruises covering her heals, and let out a sigh of relief as we would finally be left alone.
The next day was much more relaxed. I got taken off the IV and pain drip as soon as they’d let me, which I believe was exactly 12 hours after my surgery. The doctor and nurses all commented on how I hadn’t hit the button a single time to release more pain medication. I thought it was interesting that they all seemed to want to encourage me to hit it, I guess finding it unusual that I wouldn’t be quick to administer more medication than necessary. Once unhooked, I was able to carefully stand up and walk to the bathroom with a lot of assistance from my nurse. It felt good to get out of bed and move but it was definitely sobering to feel just how weak, sore, and incapable my body was. At this point my nurse offered me Motrin or Percocet to ease the pain. I told her I’d take a Motrin and she asked me my pain score on a scale of 1-10. With the level 10 pain of labor contractions still fresh in my memory, I rated myself at about a 7. “You can take a Percocet if your pain is that high,” my nurse encouraged me. “I understand, but I’m breastfeeding and don’t want a Percocet in my system.” She tried to assure me that it was “perfectly safe,” but all my mind could think about was how much more stuff had already entered McKenna’s system than I had originally desired. “I’ll stick with Motrin for now,” I reiterated.
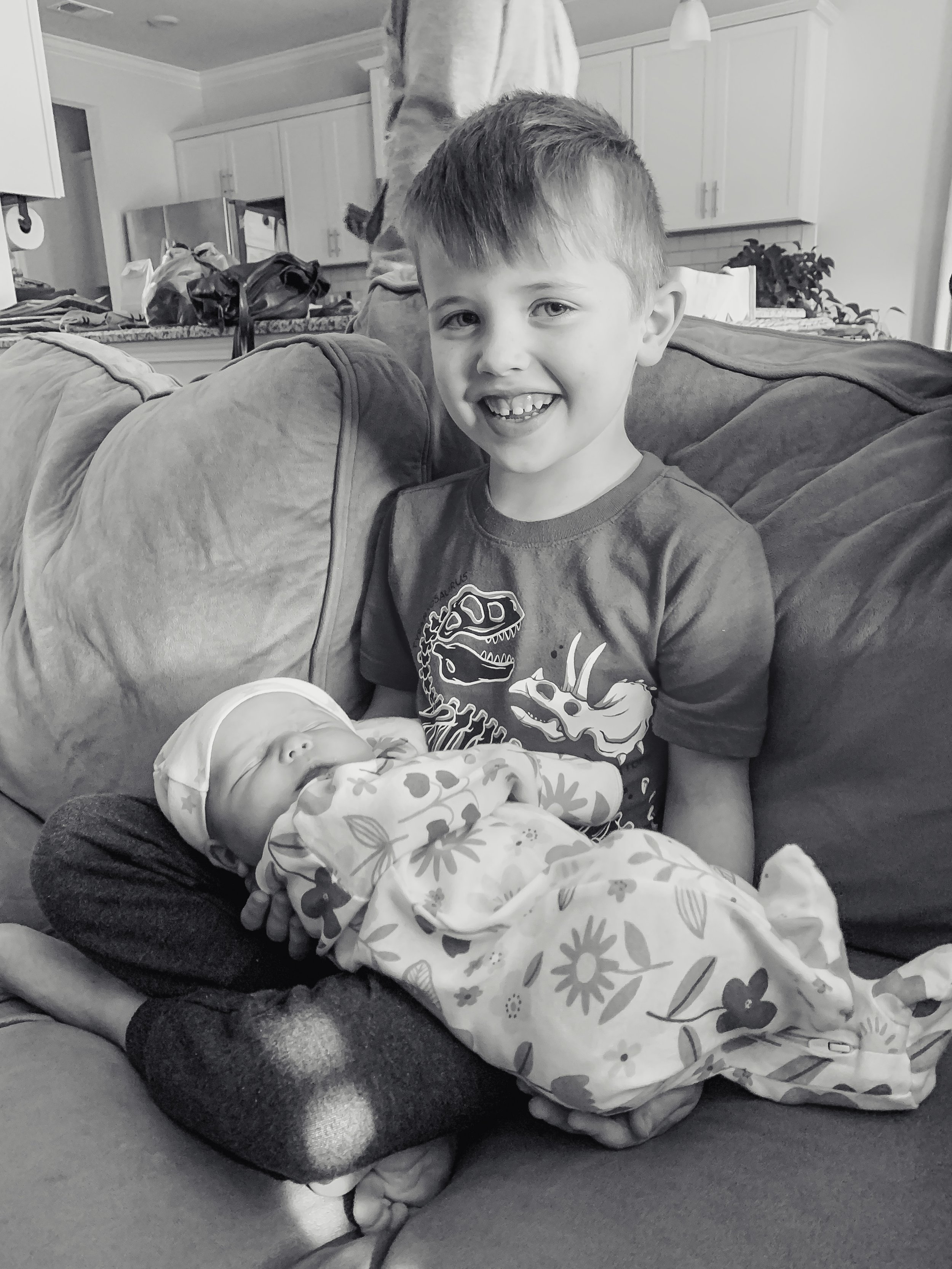
I kept on that routine for the next 36 hours. My time was filled with baby cuddles, nursing, sleeping, taking my timely Motrin doses, and slowly practicing standing up and going to the bathroom on my own. We ended up being able to leave the hospital and get home exactly 48 hours after McKenna’s birth. I’ve never been so happy to leave a place. We hurried back to our house to finally have all three of our babies at home together. Beckett and Cadence were anxiously awaiting our arrival, excited to meet their new little sister. The abruptness of having Mommy and Daddy gone in the hospital had weighed heavily on them over the last two days, as none of us had properly planned for that scenario. We were all ready to be back together again. When we finally got home, brother and sister met McKenna with complete and utter adoration. It was clear that they were immediately wrapped around her finger, and now, four weeks later, that feeling of love and infatuation has stayed with them unwavering. I feel incredibly blessed to be sitting at home with all five of us under one roof. There’s a beautiful feeling of completeness that fills my heart with peace, and McKenna has proven to be the sweetest addition to our family.
As I’ve taken the time to reflect on my birth over the last few weeks and began to share it with others, I’m sure many people assume that I regret my decision to have a homebirth, considering we ended up in the hospital with a c-section. But those people couldn’t be more wrong. I have never felt more grateful that the girl who never had a desire to birth at home decided to take a leap of faith ten months ago. The 7 hours that I spent laboring with my support team at home was the only time in my entire life that I’ve been able to experience beauty within the realm of birth. Every other birth experience I’ve had is laced with the feelings of pain, fear, and being powerless. For the first time in my birth story, I felt truly supported, seen, and empowered.
Although I know that I will need to mourn never getting that quintessential birth experience, what I did experience was potentially more profound. Seeing firsthand the stark contrast between a homebirth and a hospital birth setting within the same 12 hour period has lit a fiery passion within me that I never anticipated having. I’ve gone from being the girl who never desired to have a homebirth, to a girl who is so staunchly rooted in my desire to encourage more women to consider one for themselves - especially those women who, like me, think it isn’t for them. I saw a survey recently that concluded that nearly 50% of women identify as having birth trauma. 50 percent! And after this experience, it’s no wonder as to why. Women weren’t meant to be treated inhumanely during birth. We weren’t meant to be seen as just another number filing in and out of a patient room assembly line, with our voices stripped away so that a checklist of protocols can be marked as complete. We weren’t meant to then be handed a newborn and ushered out the door, unsure of how to breastfeed or how to heal, with no one scheduled to check in on us for another 6 weeks. It wasn’t meant to be this way. And as I’ve come to learn, with homebirth it doesn’t have to be.
During my two week follow up, my doula shared with me a quote that stated, “A hospital transfer isn’t a failed homebirth, it’s just a good use of resources,” and after experiencing it myself, I couldn’t agree more. Contrary to what many people probably believe, the success of homebirth isn’t solely rooted in the physical birth of a child, but rather it is equally rooted in the successful and gentle care-taking of the mother. It is an experience that goes way beyond the measure of a physical birth, and branches into the spiritual and emotional wellbeing of everyone involved. It’s no wonder that this is the first birth I haven’t felt the mark of trauma from, even with all of its unpredictability. Because through every twist and turn I felt the comfort and safety of those who were in my corner, helping me every step of the way, invested in my birth almost as much as I was. Now going forward, feeling that level of care, support, and love is something that I hope many more women can feel during their birth experiences, and I hope that I can be a small part of bringing about the much needed change that makes positive birth experiences the norm in our culture.